TMS Therapy | Denver & Golden

What is TMS?
Transcranial Magnetic Stimulation (TMS) is an innovative and non-invasive therapy to treat conditions such as depression, anxiety, OCD, and smoking cessation.
How Does TMS Work?
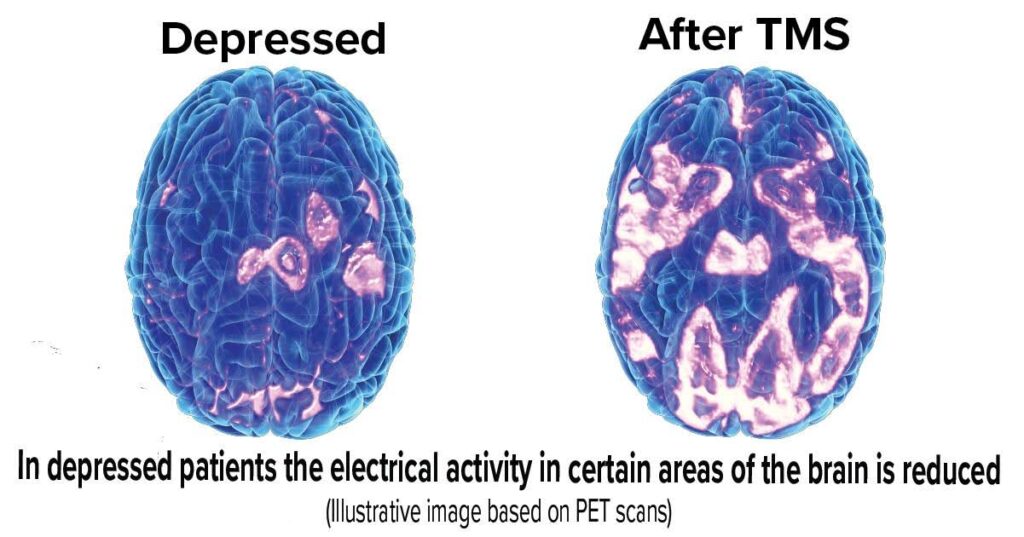
TMS uses magnetic fields to electrically stimulate nerve cells in specific parts of your brain, which has been shown to improve mental health. There are various types of TMS but most of them target the prefrontal cortex. During treatment, a patient sits in a chair, similar to at a dentist’s office, and a machine with a specific type of coil is placed by the patient’s head. Some devices will have the patient wear a cap that has the child in it where other devices can place the coil close to the patient’s head. The machine then induces hundreds to thousands of magnetic pulses through the coil to stimulate the brain area that has been targeted for depression, anxiety, OCD, or smoking cessation. There are trials underway for more uses of TMS including PTSD, bipolar, psychosis, and other addictions.
Types of TMS Therapy
There are several types of TMS therapies and protocols that can be used. A standard TMS is 5 days per week for 4-6 weeks, and the sessions last 20-60 minutes. There are newer protocols that can be done over much shorter sessions (3 minutes/session) and the entire treatment course done over the course of a single day. Different types of TMS include single vs paired pulses, rTMS (repetitive TMS), TBS (Theta Burst Stimulation), dTMS (deep TMS), iTBS (intermittent Theta Burst TMS), aTMS (accelerated TMS), and nTMS (navigated TMS). The type of TMS you would receive depends on the type of machine being used and the psychiatric evaluation and treatment plan to determine the best treatment course for your condition.
See below to see the types of TMS offered at A Better Day Psychiatry.
Who is a Good Candidate for TMS?
TMS can be a great treatment choice for most people with depression, anxiety, OCD, or wanting to quit smoking. It has success rates of 40-80% for conditions such as depression and anxiety, which is comparable to or better than what is achieved with medications, so patients who do not want to be on a psychotropic medication or have failed psychotropic medications may be good candidates for TMS. A major factor for most people for TMS relates to if it will be covered by insurance or not, which will be covered below. Lastly, TMS is mostly contraindicated if the patient is pregnant (or planning to be pregnant soon), has a seizure disorder, or has metal devices in their head or some other medical devices in their bodies such as a pacemaker, does not have active symptoms of psychosis, mania, or suicidality, and is between 18-70 years old though those age ranges will .likely be expanded soon by the FDA.
What Are the Requirements for TMS Therapy?
Requirements for TMS are primarily dictated by insurance companies and the evaluation of the TMS provider/psychiatrist. If a patient is paying out of pocket, then most of these requirements do not apply. Each insurance may have different criteria for covering TMS but in general they need a diagnosis from a psychiatrist for Major Depressive Disorder, Anxiety with Depression, or OCD as those are what are currently indicated uses by the FDA (including smoking cessation). They likely will need to have failed at least two medications to treat these conditions, and they should have impairments in their life from these conditions. The patient would need a psychiatric evaluation to demonstrate they meet these criteria.
TMS Therapy Results
TMS therapy has results ranging from 40-85% with the best results (in the 80+% range) from rTMS, dTMS, and aTMS (or rapid, deep, or accelerated TMS). The type of machine being used will determine if these modalities can be done. At ABD, we are able to do both rTMS and aTMS through the Magstim 3.0 device.

The device we use
(Magstim Horizon 3.0 with Stimguide)
and benefits around this device
A Better Day Psychiatry uses the Horizon 3.0 with Stimguide (navigation guidance).
Through integrated guidance, we achieve:
- Shorter pulse widths for less discomfort
- Improved Coil Positioning for accuracy and repeatability of pulses
- Reduced risk of off-target stimulation
- No “pulse decay” – delivering consistent doses
- Data analytics to monitor treatment progress
- A wide range of TMS protocols including rTMS, TBS, iTBS, and aTMS.
This device has FDA clearance for Major Depressive Disorder, Anxious Depression symptoms, and OCD.
Our process for TMS at A Better Day Psychiatry
Initial free 15-minute consultation
We suggest for anyone considering TMS to book a free 15-minute consultation to see if you would be a good candidate for TMS and to explain the process.
Psychiatric Evaluation before beginning TMS
If proceeding with TMS, we start with a full psychiatric evaluation. This process will ensure that a thorough psychiatric and medical history is performed to make sure you are a good candidate and to rule out any contraindications to TMS (see FAQ). If the provider and patient decide TMS is not the best option moving forward, the psychiatric evaluation will still include treatment recommendations including lifestyle modification recommendations, therapy, and medications.
Monitoring Progress Through Treatment:
We monitor progress with a combination of rating scales every two weeks as well as check-ins with your provider anywhere from weekly to every 2-4 weeks depending on the presenting symptoms. The rating scales will provide an objective measure to monitor progress and efficacy over the course of the treatment.
Completion of TMS:
After completing the full course of TMS, there will be a check in with your provider to assess how the treatment went and to formulate a plan for after treatment. Assuming there was improvement in symptoms, this can be a great opportunity to reassess someone’s medication regimen, review coping strategies, and encourage healthy lifestyle changes. In some cases, patients can have a recurrence of symptoms after 6+ months and those patients can respond well to maintenance TMS.
TMS Therapy Pricing
Please call our office for more detailed information about pricing, insurance, financing, and out-of-pocket packages.
Intake evaluation
with Psychiatrist ranges depending on the provider
$250-$450
TMS Session
per session fee
$200-$300
In most cases, this will be covered by insurance, but we will need to work with your insurance beforehand to get it approved.
*Payment plans available including financing and discount on payment in full
Patient Stories:


TMS Therapy FAQs
Is TMS Therapy Permanent?
TMS is not considered curative but in most cases can provide lasting relief from depression, anxiety, OCD, etc. and in some cases longstanding remission. Approximately 50% of patients may experience some recurrence of their symptoms after 6 months, but this can be a critical window of time to implement other coping strategies and support.
What Part of the Brain Does TMS Target?
TMS generally targets the prefrontal cortex. At ABD we target the dorsolateral prefrontal cortex through the Horizon 3.0 with StimGuide Pro. The Stimguide allows us to ensure precise delivery of the electromagnetic pulses to the dorsolateral prefrontal cortex and at the end of each session it shows a report if any pulses were missed so they can be implemented again.
How Long Do the Effects of TMS Treatment Last?
TMS typically lasts 6+ months. For patients who have a recurrence of symptoms after 6 months, there is the option for maintenance treatments.
Does TMS Help with OCD?
TMS has been FDA indicated for OCD. It can depend on the device being used though if that specific device has been approved by the FDA. Fortunately at ABD, our device the Magstim Horizon 3.0 is FDA indicated for OCD. TMS can help reduce the frequency and intensity of obsessions and compulsions.
Does TMS Work for Depression?
As above, TMS is only FDA indicated for Major Depressive Disorder on certain devices, but our device at ABD has been approved by the FDA. TMS has been shown to lead to a greater than 50% reduction in symptoms in 50% of patients and leads to full remission from depression in 33% of patients.
Is TMS Effective for Anxiety?
TMS has been FDA indicated for “anxious depression” or patients who have Major Depressive Disorder with anxious features. Similar to depression, most patients experience a greater than 50% reduction in symptoms of anxiety from TMS.
Is TMS painful?
The most common side effects of TMS include headaches, discomfort in the scalp, muscle twitches, or dizziness/lightheadedness. Rarely people can experience syncope (fainting such as after a blood draw) or mood changes. Very rarely (roughly 1 in 30,000 people) can experience seizures. The side effects can be greatly reduced by the type of TMS and device being used. At ABD, we use a navigation-guided device as well as place electrodes on the thumb to measure the motor threshold to ensure the side effects are as minimal as possible.
