How does marijuana impact antidepressants? Mixing marijuana and antidepressants is complex and the current research is limited. With an increase in usage of both marijuana and antidepressants, it comes as no surprise that patients are increasingly wanting to learn more about the interaction between the two. This article explores these intricacies in an explanation on how using marijuana impacts antidepressants.
TABLE OF CONTENTS
How Does Marijuana Impact Antidepressants
The Effects of Marijuana on Antidepressant Efficacy
Types of Antidepressants and Their Interaction with Marijuana
SSRIs: The Interaction with Cannabis
SNRIs, MAOIs, and Tricyclic Antidepressants: The Interaction with Cannabis
MAOIs: The Interaction with Cannabis
Tricyclic Antidepressants: The Interaction with Cannabis
Potential Risks and Side Effects of Combining Marijuana with Antidepressants
How Does Marijuana Impact Antidepressants?
Patients are increasingly interested in learning about how does marijuana impact antidepressants. Common questions include:
- Is smoking marijuana safe while on an antidepressant?
- Can I use cannabis while on medications like Lexapro or Zoloft?
- What happens if I combine marijuana with my antidepressant?
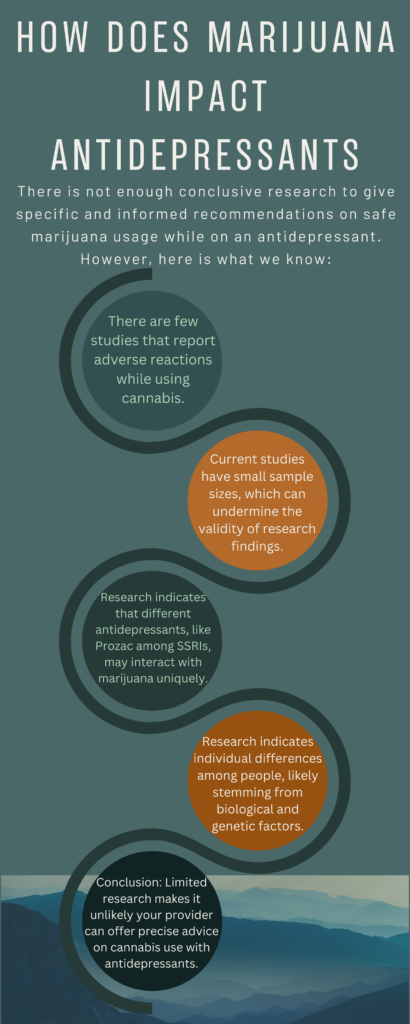
The short answer is that there is currently not enough high-quality research to definitively determine whether using marijuana while taking antidepressants is safe. Available data suggest that interactions vary based on multiple factors, including the class of antidepressant, dosage, frequency of cannabis use, individual metabolism, and genetic differences. Because of this variability, the effects can be unpredictable from person to person.
Before focusing solely on safety, what is even more important is open communication with your mental health provider. It is essential that your psychiatrist or psychiatric provider is aware of how often and how much marijuana you use so they can provide individualized, evidence-based guidance. A quality provider will approach this conversation without judgment and help you weigh potential risks and benefits within the context of your treatment plan. At A Better Day Psychiatry, our providers are knowledgeable about the evolving research on cannabis and antidepressant interactions.
Cannabis interacts with neurotransmitter systems involved in mood regulation, including serotonin and dopamine, which are also targeted by many antidepressants. Because of this overlap, marijuana use may influence how antidepressants work in the brain.
Responses to cannabis can also vary depending on the mental health condition being treated. Marijuana may affect depressive symptoms differently from person to person, and in some cases may worsen anxiety, mood instability, or depressive symptoms. For these reasons, individualized guidance from a mental health professional is essential.
The Effects of Marijuana on Antidepressant Efficacy
Marijuana has the potential to affect how well antidepressants work in the body. One of the primary mechanisms involves the cytochrome P450 enzyme system, a group of liver enzymes responsible for metabolizing many medications, including antidepressants.
Cannabis can inhibit certain cytochrome P450 enzymes, which may cause antidepressants to remain in the body longer than intended. As a result, medication levels can rise, increasing the likelihood of side effects. In some cases, altered metabolism may also affect how consistently an antidepressant works.
Changes in antidepressant levels may influence treatment outcomes in different ways. For some individuals, higher medication levels could increase side effects without improving symptoms. For others, cannabis use may reduce antidepressant effectiveness, potentially leading to persistent or worsening symptoms. Because of this variability, the impact on treatment response is difficult to predict.
Clinical and pharmacologic factors that may influence these effects include:
- Individual genetics and metabolism, which affect how both cannabis and medications are processed
- Medication dosage and cannabis potency, including THC concentration, frequency of use, and method of consumption
Due to these variables, mental health providers often recommend caution and close monitoring when cannabis is used alongside antidepressant medications.
Types of Antidepressants and Their Interaction with Marijuana
Different classes of antidepressant medications can interact with marijuana in different ways. Because these medications vary in how they work in the brain and how they are metabolized, drug interactions related to marijuana and antidepressants can be unpredictable.
Key differences across antidepressant classes include:
- SSRIs, SNRIs (such as Effexor XR), and tricyclic antidepressants (TCAs) may each respond differently when combining marijuana, based on clinical and pharmacologic considerations.
Individual mental health factors also play an important role. People with anxiety disorders, depression, or other mental health conditions may notice that marijuana affects mood symptoms differently. In some cases, marijuana use may worsen depression symptoms or anxiety rather than help treat depression, especially when mixing marijuana with prescribed medications.
Research on how cannabis affects antidepressant treatment remains limited and inconsistent, often relying on small studies. Because of this, providers cannot reliably predict how consuming cannabis may impact depressive symptoms, medication effectiveness, or side effects. Responses can vary based on the presence of mental disorders, use of other illicit substances, or co-occurring conditions such as chronic pain.
For these reasons, mental health providers emphasize individualized guidance and careful monitoring when patients use marijuana while taking antidepressant medications.
SSRIs: The Interaction with Cannabis
Selective serotonin reuptake inhibitors (SSRIs) are the most commonly prescribed antidepressants, which is why SSRIs combined with cannabis is one of the most frequently asked-about medication combinations. Common SSRIs include medications such as fluoxetine (Prozac), sertraline (Zoloft), and escitalopram (Lexapro). Despite how common this question is, research on the interaction remains limited and is still emerging.
SSRIs work by increasing serotonin levels in the brain. Cannabis may interfere with how these medications are metabolized, which can potentially raise SSRI levels in the body. In rare cases, this may increase the risk of serotonin syndrome, a potentially serious condition caused by excessive serotonin. Symptoms can range from mild (agitation, sweating, tremor) to severe (confusion, seizures, or loss of consciousness).
Current research on SSRIs and cannabis consists largely of small studies and case reports. Some evidence suggests that cannabis use while taking an SSRI may increase anxiety or panic symptoms in certain individuals, though these findings are not conclusive and require further study.
Potential considerations include:
- Mixing marijuana or combining marijuana with SSRIs may increase the risk of side effects due to changes in medication levels.
Cannabis may also affect depressive symptoms differently in people taking SSRIs. While some individuals report temporary symptom relief, others may experience worsening mood, increased anxiety, or emotional blunting.
Because responses vary and high-quality data is limited, mental health providers typically recommend caution, ongoing monitoring, and open discussion when cannabis is used alongside SSRI medications.
SNRIs, MAOIs, and Tricyclic Antidepressants: The Interaction with Cannabis
While SSRIs have received the most attention in research, other classes of antidepressants also interact with marijuana in unique ways. Evidence is limited, and much of what is known comes from small studies or case reports, so responses can vary widely depending on individual factors and how cannabis is consumed.
SNRIs: The Interaction with Cannabis
Serotonin-norepinephrine reuptake inhibitors (SNRIs), such as Effexor XR and duloxetine (Cymbalta), increase levels of serotonin and norepinephrine in the brain. Cannabis may affect the metabolism of SNRIs, leading to higher or lower medication levels in different people.
- Potential drug interactions can alter the effectiveness of the SNRI or increase the risk of side effects, including anxiety or nausea.
MAOIs: The Interaction with Cannabis
Monoamine oxidase inhibitors (MAOIs) work by preventing the breakdown of neurotransmitters like serotonin, dopamine, and norepinephrine. These medications are less commonly prescribed due to higher interaction risks.
- Higher interaction risks exist when combining MAOIs with cannabis or other illicit substances, which may lead to unpredictable reactions.
Tricyclic Antidepressants (TCAs): The Interaction with Cannabis
TCAs, such as amitriptyline (Elavil) and nortriptyline (Pamelor), increase serotonin and norepinephrine levels similar to SNRIs. Cannabis use may alter the metabolism of TCAs and increase the likelihood of side effects.
- Possible cardiovascular effects, including tachycardia or irregular heartbeat, have been reported in limited studies.
It’s important to note that how cannabis is consumed, including dose, potency, and frequency, can influence the severity of these interactions. Individual factors such as genetics, mental health history, and concurrent use of other medications also contribute to variability in response.
Potential Risks and Side Effects of Combining Marijuana with Antidepressants
Research on the risks of combining marijuana with antidepressants is limited, and much of what is known comes from small studies and case reports. However, available evidence suggests several potential risks and side effects may occur when marijuana is used alongside antidepressant medications.
Possible risks include:
- Rare but potentially serious reactions, including serotonin syndrome, particularly with certain antidepressants
- Increased side effects of antidepressants, as marijuana may raise medication levels in the body
- Fatigue, dizziness, diarrhea, cough, or nausea
- Increased anxiety or panic attacks, which has been reported in limited case studies
- Cognitive changes, such as impaired attention, confusion, or slowed thinking
- Mood changes, including irritability or emotional blunting
- Worsening depressive symptoms in some individuals, even if marijuana initially seems to help
For individuals using cannabis to manage chronic pain, combining marijuana with antidepressants may increase the likelihood of side effects, as both can affect the central nervous system and overall alertness.
Cognitive and mood-related side effects may be more likely with high-potency THC products, higher doses, or frequent use.
Responses vary widely based on individual factors such as genetics, mental health history, dosage, and frequency of use. Because of this variability, mental health providers typically recommend caution, monitoring, and open discussion when marijuana is used during antidepressant treatment.
Conclusion
In summary, research on marijuana and antidepressants remains limited, and clear answers about safety and effectiveness are still lacking. While significant interactions appear to be uncommon, the available evidence shows that responses can vary widely and are difficult to predict.
Open communication with your mental health provider is essential, particularly as part of effective medication management. If you use marijuana while taking antidepressant medications, it’s important to monitor for changes in depression symptoms, anxiety, mood, or overall functioning, particularly for individuals with anxiety disorders or other mental health conditions.
Key takeaway:
- How cannabis affects antidepressant treatment can differ significantly based on dosage, frequency of use, and the class of antidepressant medication.
Most importantly, discussions about marijuana use should feel safe, non-judgmental, and informed. A provider who understands potential drug interactions can help you weigh risks, monitor symptoms, and make thoughtful decisions that support your mental health and treatment goals.

