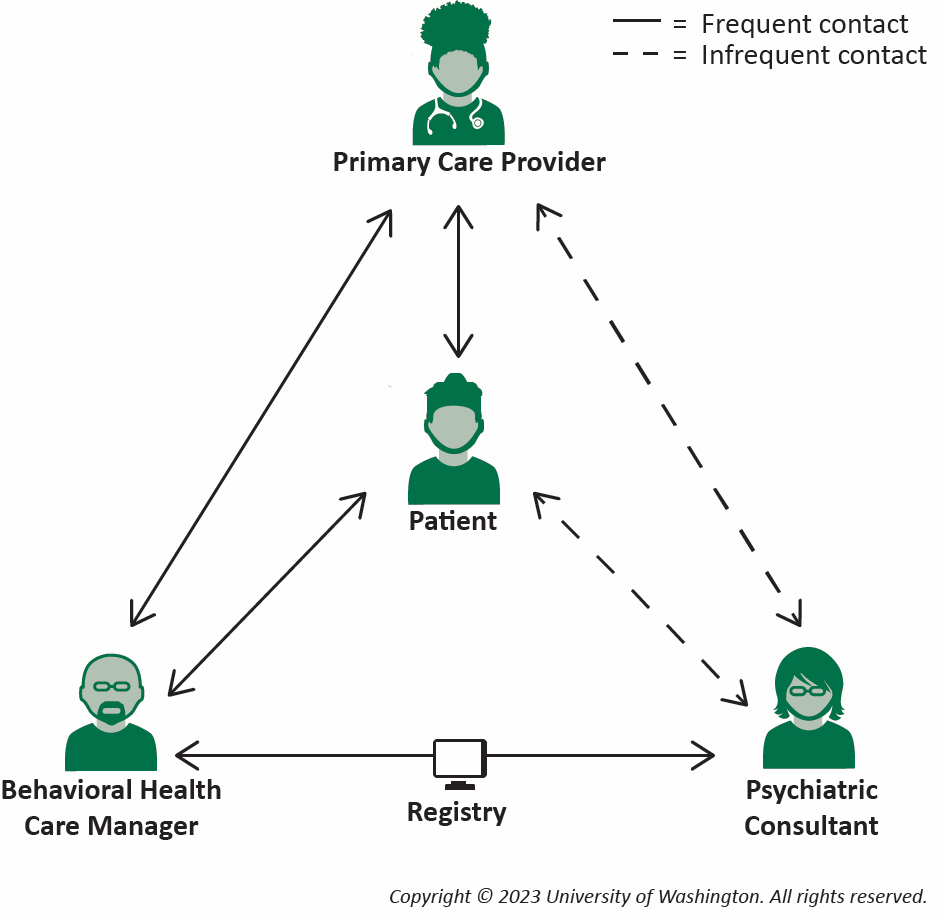
The Collaborative Care Model (CoCM) is a proven, team-based approach that integrates mental health services into primary care, making psychiatric care more accessible and effective. In this model, primary care providers, behavioral health care managers, and consulting psychiatrists work together to deliver evidence-based treatment for common mental health conditions like depression and anxiety. By leveraging a structured system of care coordination and measurement-based treatment, CoCM improves patient outcomes, increases access to psychiatric expertise, and enhances overall efficiency in healthcare settings. This model is particularly effective because it meets patients where they already receive care—reducing stigma, addressing mental health concerns earlier, and ensuring a seamless connection between physical and mental healthcare.
Key Components of CoCM
The Collaborative Care Model utilizes a team composed of a primary care provider, a Behavioral Health Care Manager, and a psychiatrist to discuss a patient with mental health issues. The PCP and BHCM describe the case to the psychiatrist, who provides evidence-based recommendations for the PCP to implement. This team then continues to meet to review the case over time until the patient is stable, and the PCP can take back over the case.
Benefits for Patients & Providers
- Discuss improved mental health outcomes, accessibility, and efficiency.
- The CoCM has over 90 randomized controlled trials demonstrating that it is the integrated care method with the most evidence backing its use. These trials demonstrate improved clinical results, enhanced patient and provider satisfaction, and decreased medical expenses. Providers are able to grow their knowledge base for managing mental health disorders while patients receive care from a specialist but in the primary care setting.
How the Collaborative Care Model Works at Our Practice
At A Better Day Psychiatry, we work with primary care practices to increase their knowledge base and provide mental health expertise for their patients. We typically meet anywhere from weekly to monthly with the behavioral health care manager and PCP to discuss cases and develop a comprehensive treatment plan together. We provide a detailed rationale for why we are choosing this treatment plan and see it as an opportunity to educate and empower these practices to manage more mental health issues that come up for their patients on their own. For patients who are too complex for primary care, we can see those patients in our clinic or remotely and take over their mental health care until they are stable then transition them back to their primary care team.
Challenges & Solutions
The biggest challenge with the CoCM involves how new it is, increasing awareness of it to practices through the state, and then getting reimbursed through insurance companies for the cases discussed.
Why Providers Should Consider a Collaborative Care Model (CoCM)
- Professional development for primary care teams and increasing their comfort and knowledge managing complex mental health issues guided by a double boarded adult and child/adolescent psychiatrist.
- Increased access to mental health care for patients
- More effective and efficient care
- Decreased healthcare costs managing mental health issues in primary care rather than higher acuity settings
- CoCM and Psychotherapy Billing codes through insurance to provide reimbursement to the PCP offices PER PATIENT discussed in the meetings
- At A Better Day Psychiatry, we believe in increasing access to mental health treatment and partnering with primary care to achieve this. Reach out to our team of providers to learn more!

